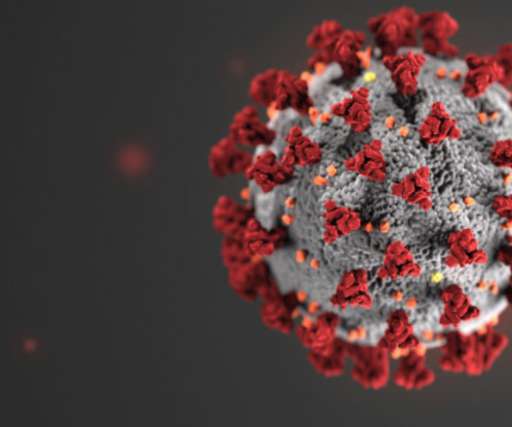
The Changing Face of Healthcare Amidst the COVID-19 Pandemic
Hospital Recruiting | Nursing
APRIL 1, 2020
Remote Patient Care In this age of social distancing, telemedicine has come out on top. The emergency decision by the Center for Medicare and Medicaid Services (CMS) on March 17, 2020 (and retroactively in effect beginning March 6, 2020) to pay for telehealth visits outside of rural areas has eased physician concern.



















Let's personalize your content