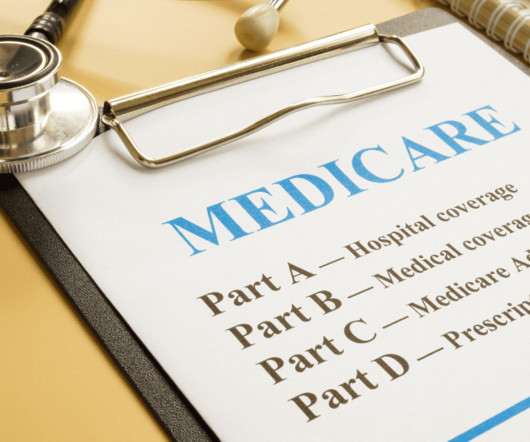
Enhancing Patient Advocacy and Care through Medicare Fluency
American Nurse
SEPTEMBER 6, 2024
This gap can be vast when patients are unaware of the Medicare benefits available or do not understand how to access these benefits effectively. Nurses with a solid understanding of Medicare can: Educate patients on the importance of preventive services covered by Medicare, leading to early detection and better outcomes.










Let's personalize your content